Abstract: The U.S. Patient Protection and Affordable Care Act (ACA) mandates that COPD patient readmissions to a hospital that exceed a predetermined threshold in less than 30 days from discharge will result in financial penalties to the involved institution.1 COPD patient readmissions prevention has been hampered due to an inadequate understanding of the underlying problems facing both the patient and the health care provider. There are many transition-to-home challenges and other “disconnects” that occur across the continuum of care. Most current models of care rely solely on the use of various types of medications and devices in an attempt to achieve the desired clinical outcomes, ignoring the chronic and behavioral components of the disease. A new model of care is needed to focus on practical, simple and affordable solutions to this problem. The purpose of this paper is to critically review the current methodology with its advantages and deficits and provide a fresh look at the cause and prevention of COPD hospital 30-day readmissions.
INTRODUCTION AND OVERVIEW
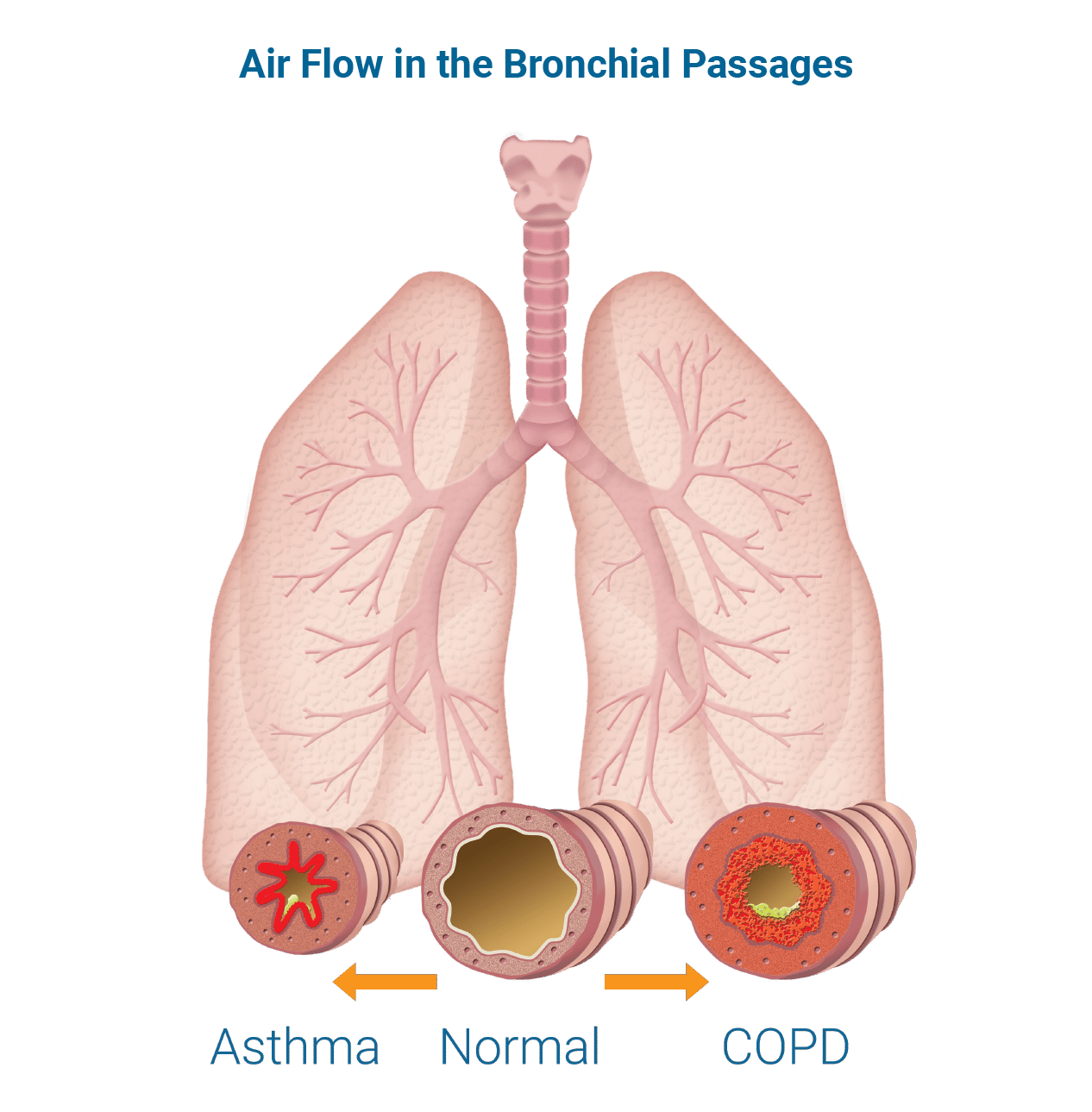
Chronic Obstructive Pulmonary Disease (COPD) is the third leading cause of death worldwide.2 The magnitude of the problem is increasing now that baby boomers have reached the prime age of COPD disease manifestation. COPD is a chronic and progressive lung disease that, in later stages, is associated with acute exacerbations (flare-ups) that often occur with increasing frequency and intensity. While there is no cure for COPD at this time, most aspects of the disease are treatable. The current healthcare delivery model treats patients with COPD primarily when they present in an acute phase of the illness, but very few patients receive active management for the chronic component. Such a “disconnect” may be related to the U.S. national average 30-day readmission rate of 23% for patients who are hospitalized with a COPD exacerbation.3 In an attempt to reduce health care costs under such circumstances, the U.S. Centers for Medicare and Medicaid Services (CMS) has intervened by creating financial disincentives related to hospital reimbursement.
Through the ACA, CMS has introduced 30-day readmission reimbursement penalties. These penalties are geared to begin the process of moving from a “fee-for service” model in which transitions between acute and chronic disease states can be disconnected, to a patient centric, disease management system in which care is coordinated across the acute and chronic phases. In a disease management system, the patients are trained and supported as they learn to participate in the management of their illness. The ultimate goal is to reduce the occurrence and re-occurrence of exacerbations requiring multiple hospitalizations. The purpose of this white paper is to describe the causes of unacceptably high 30-day readmission rates and to identify the principles and components of a methodology to prevent COPD patient readmissions.
This white paper draws upon the experiences of an expert panel, as well as conclusions from clinical trials that have addressed the 30-day readmission problem and associated behavioral issues related to the need for pulmonary rehabilitation.
The expert panel includes Brian Carlin, M.D., Brian Tiep, M.D., Trina Limberg, RRT, MAACVPR, and Robert McCoy, RRT, FAARC.
Dr. Carlin is a pulmonologist in Ingomar, PA, vice-chair of the American College of Chest Physicians, and past president of the American Association of Cardiovascular and Pulmonary Rehabilitation. He has assisted with the development of two pilot projects that reduced COPD 30-day readmissions from an average of 23% to 5% following the intervention.4
Dr. Tiep is the Director of Pulmonary Rehabilitation at City of Hope Medical Center in Duarte, CA and Medical Director of the Respiratory Disease Management Institute in Monrovia, CA. He has published articles on pulmonary rehabilitation disease management, and co-authored the American Thoracic Society/European Respiratory Society 2004 Standards for the Diagnosis and Treatment of Patients with COPD. He has been treating COPD patients for more than 40 years, and his program has a 4% admission rate for COPD exacerbations.5 He holds over 15 patents associated with respiratory care.
Trina Limberg, RRT, MAACVPR, is the Director of Preventative Pulmonary and Rehabilitation Services at University of California at San Diego. She is a Master Fellow of the American Association of Cardiovascular & Pulmonary Rehabilitation, has served on numerous consensus panels and has more than 30 years of experience treating COPD patients.
Robert McCoy, RRT, FAARC, is General Manager of Valley Air Respiratory Services in Minneapolis, Minnesota, where he conducts clinical research and testing, and is a program development consultant.
This panel has also reviewed a number of programs and case studies that have reduced readmissions rates, such as the DASH (Discharge Assessment and Summary at Home) program, Klingensmith HealthCare, Ford City, PA4 and the University of California Davis Medical Center ROAD (Reverse Obstructive Airway Disease) COPD action plan.6 In addition, the panel has evaluated studies in aligned areas and disciplines in order to identify clinical tools that may be helpful to address the 30-day readmission problem.
WHAT ARE THE CAUSES OF HIGH COPD 30-DAY READMISSION RATES?
Exhibit I depicts the exacerbation cascade. Exhibit II (see page 6) details the treatment challenges associated with enabling COPD patients to avoid exacerbations and exacerbation relapses resulting in 30-day readmissions. Those challenges can be summarized into six categories:
1. Exacerbations are frequently not fully resolved at the time of discharge. An inadequately treated exacerbation leaves the patient vulnerable to relapse.
2. Disjointed patient management occurs across the continuum of care. The current system of provision of care often results in care fragmentation, such that the providers for each step of care (e.g., outpatient primary care physician, emergency department, hospitalist) are not sufficiently coordinating the overall management of an individual patient. Often there is no designated coordinator following the patient throughout the care plan. This lack of continuity can result in a “discontinuum of care” in which recovery from the acute phase is not completed, and/or the chronic component of the disease is not managed. The result can be a relapse and readmission, or an admission within 30 days due to a new exacerbation or an associated comorbidity.
3. Patient training is inadequate. Studies show that when patients get home, they may not remember a significant amount of information that was provided during the discharge process.7 And, with a lack of post-discharge follow-up by healthcare providers, a number of vital treatment steps can fall through the cracks. For example, patients may not administer medications correctly; they may not have their oxygen, or be sufficiently oxygenated; they may have resumed smoking; and they may remain sedentary. The patient activity plan (which is vital to airway clearance, patient conditioning and early recognition of a worsening condition) may not be followed. In addition, saturation monitoring and airway secretion clearance steps may not be followed. These lapses can lead to a worsening of the COPD and, ultimately, readmission.
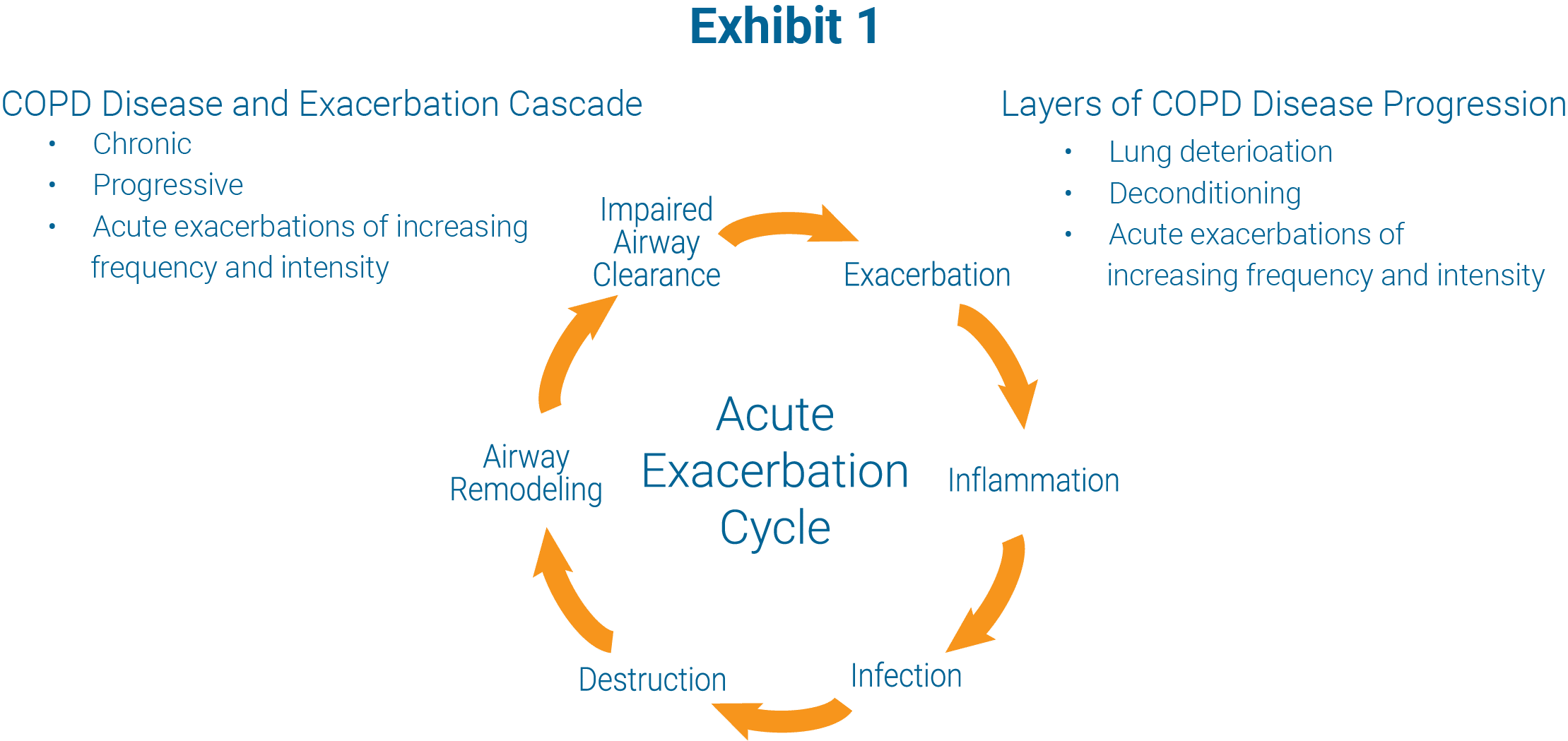
Disclaimer: It is understood that not all exacerbations progress in this manner or lead to tissue destruction or remodeling (change in tissue structure or morphology).
4. Lack of professional follow-up care occurs post discharge. 75% of patients being readmitted within 30 days have not seen their primary care provider.3 Additionally, home respiratory care provided by a professional respiratory therapist in the COPD patient’s home is not reimbursed and therefore not typically provided. Without this critical evaluation of the patient in their environment, disconnects in treatment are not rectified and the patient will risk having a relapse and readmission. And, competitive bidding has made it much more difficult for homecare companies to be able to provide those services.
5. Equipment in the home is inadequate. Reimbursement reductions are resulting in some homecare providers having to source less expensive equipment and/or equipment requiring fewer home service calls. For example, some patients may receive delivery systems that are not practical for ambulatory use such as an E-cylinder which can weigh as much as 22 lbs. and may be too heavy for a weak and debilitated patient. Additionally, some patients with high flow supplemental oxygen needs may be inadequately oxygenated by some of the portable systems in use. Both of these examples can be an impediment to the patient being active. Activity is vital to the patient’s care plan. Equipment alone cannot accomplish clinical outcomes and variable/limited equipment may mask the cause of an exacerbation.
6. Lack of an exacerbation Rapid Action Plan. Exacerbations are usually addressed too late in their course so that by the time the exacerbation is detected the inflammatory and destructive processes that are part of the exacerbation are well developed. Additionally, patients who go to the Emergency Department (ED) often experience significant delays in the initiation of treatment, leaving the exacerbation, and its associated inflammatory and subsequent destructive process, unattended at a critical and vulnerable time. The concept here is captured in the phrase “time is tissue”. If exacerbations are recognized early and treated promptly, re-hospitalization may be averted.
PRINCIPLES OF A PATIENT-CENTERED, CROSS-CONTINUUM, DISEASE-MANAGEMENT APPROACH TO REDUCING COPD 30-DAY READMISSIONS
Traditional care plans draw a distinction between treatment (acute) and prevention (chronic). In fact, both should be addressed in the overall management of the COPD patient. A strategy is needed that encompasses the tools to address the disease characteristics, presentation, and patient response — both physiological and behavioral. This panel has drawn on the successes of recent case studies as well as their own experiences to develop a plan of care to reduce COPD patient 30-day readmissions. The following is an overview of the principles of that program.8,9
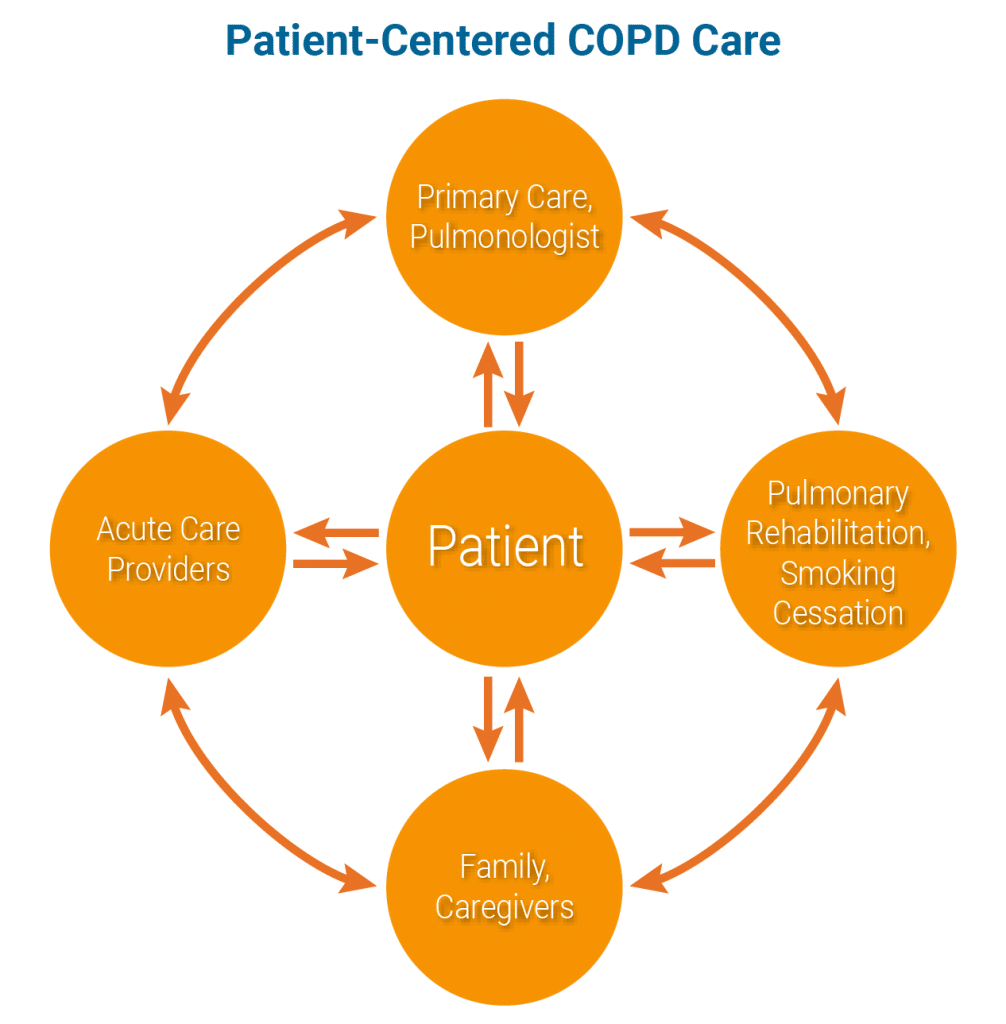
1. Cross-continuum of care delivery. Manage the chronic as well as the acute phases of the disease. This requires a team that coordinates across the care continuum ensuring smooth transitions and seamless continuation of the treatment plan.
a. COPD Coordinator function – this function plays a dual role in seamlessly transitioning the patient from the acute through the chronic phases. The first Coordinator role is one of educating and training the patient and family to self-monitor and self-manage post discharge. A Pulmonary Rehabilitation Respiratory Therapist will have many of the skills required of this function. The second Coordinator role is an “extender” of the pulmonologist; able to work across the continuum of care, particularly post-discharge, and potentially including prescribing medications and ordering therapy, with the goal being rapid response and relapse avoidance.
 b. Efficient and effective communication between the care providers (including the primary care physician, the ED physician, hospitalist, and pulmonologist).
b. Efficient and effective communication between the care providers (including the primary care physician, the ED physician, hospitalist, and pulmonologist).
c. Seamless discharge – ensure there is no interruption in the medications and care plan from the hospital to the home.
d. Home visit – shortly after discharge to assess the home environmental factors affecting the patient’s ability to adhere to a treatment regimen.
i. Proper equipment – adequacy of home oxygen equipment for oxygenation (titration) and mobility.
ii. Medication reconciliation – ensure that medications prescribed by multiple MDs are reconciled.
iii. Continue smoking cessation, assuring the availability and use of medication.
iv. Cognitive, family and financial considerations.
2. Patient-centered care. Patient involvement in the delivery of their care is central to the successful management of this progressive disease with chronic and acute phases. Patient training in self-monitoring and self-managing as well as early recognition and response to exacerbations brings this concept to life. There is a need for a mechanism for patient collaboration with the healthcare providers.10
3. Active lifestyle. The centerpiece of successful COPD management.
a. Inactivity is destructive.
b. Activity supports overall physical and mental health, supports airway clearance and helps with early exacerbation recognition and rapid response.
4. Patient training. Use of the “teach-back” method, in which the patient “teaches” the clinician, enables the patient to self-monitor and self-manage while collaborating with the healthcare provider. Pulmonary rehabilitation and patient training begins at the “inpatient” stage and is reinforced after the patient is discharged. The patient should have a checklist of responsibilities and daily activities.
a. Proper administration of home meds, particularly inhaled medications.
b. Mobility and exercise – usually walking.
c. Titration of home oxygen equipment – adjusted per SpO2 monitoring.
d. Pursed-lips breathing – may use pulse oximeter as a biofeedback guide to increasing SpO2.11
e. Airway clearance.
f. Avoidance of smoking and exposure to second hand smoke.
g. Avoidance of exposures to toxic perfumes, dusts, chemicals.
5. Proper equipment. A requirement for success.
a. Metered Dose Inhaler spacer for improved administration of home medications.
b. Oxygen equipment titrated via pulse oximetry to ensure oxygenation as well as mobility — vital to an active lifestyle.
c. Pulse oximeter for patients with oxygen desaturation. This is useful in physician-directed oxygen titration as well as a biofeedback guide for pursed lips breathing.11
d. Airway clearance devices.
6. Rapid Action Plan. Early intervention is the key to successful exacerbation resolution and relapse avoidance.
a. Patients should be trained to recognize the early signs of an exacerbation or an exacerbation relapse. This includes greater than usual dyspnea upon the same exertion and change in sputum. When recognized, the Rapid Action Plan begins: call doctor; start steroids, antibiotics, bronchodilators and fluids; adjust oxygen; and engage in pursed lips breathing.
b. A checklist-procedure should be in place for specific interventions by the patient, physician, ED physician, hospitalist, and COPD coordinator.
c. Begin medications with many patients as early as possible, including while they’re still at home. Have medications on-hand. Time is tissue.
7. Pulmonary rehabilitation, smoking cessation. Since the patient is experiencing the worst aspects of the disease in the hospital, this is likely to be a “teachable moment.” Smoking cessation (including medications) and pulmonary rehabilitation should start in the hospital. Generally recommended for smoking cessation is either Chantix or nicotine replacement therapy with nicotine patch and a rapid acting nicotine replacement, like gum or a lozenge.
SUMMARY
In summary, successfully instituting a plan of care that will ultimately lower the COPD patient 30-day readmission rate positions the healthcare provider and system to succeed in this new, pay-for-performance healthcare paradigm. Successful management of the COPD patient embodies healthcare’s “Triple Aim” — outcomes are improved, per capita costs are lowered and people living with COPD can experience fuller, longer, and more active lives.
Exhibit II
COPD TREATMENT CHALLENGES: PROBLEMS WITH USUAL CARE MANAGEMENT
Acute:
- Active treatment occurs only during acute exacerbation.
- Time-sensitive treatment is frequently delayed.
Chronic:
- The chronic component often is not addressed.
- Even when the patient gets pulmonary rehabilitation, it is a short-term solution for a problem that is lifelong, progressive and gets worse over time.
- How patients manage their care at home can make the greatest difference in disease control.
A COPD exacerbation is a dynamic process leading to destruction and airway remodeling. Thus it is time sensitive (time is tissue). When destruction occurs, repair takes longer and tissue may not fully repair. This can lower the baseline status, rendering a future exacerbation more likely.
FACTORS CONTRIBUTING TO HOSPITALIZATION AND READMISSIONS
Lack of predetermined Rapid Action Plan:
- Symptoms are unrecognized or may be ignored for days or more.
- Lack of early access to a physician.
- Delayed response can lead to tissue destruction, airway remodeling and progression beyond simple control.
Emergency Department response:
- Response can often be inadequate because there are treatment delays or there can be insufficient treatment intensity. When treated promptly, admission/ readmission of the COPD patient can be avoided.
- Steroid treatment is often too little, too late and, as a result, too long. Thus side effects of long-term steroid use become more likely.
- There is often a delayed start for IVs, steroids, antibiotics and/or bronchodilators. To avoid treatment delay, it is important to educate the Emergency Department that active treatment can often start prior to arterial blood gas draws or chest x-rays.
In-patient treatment:
- Treatment (particularly respiratory therapy and secretion mobilization) may commence slowly, lack intensity, or be delayed.
- Patients often are not ambulated (mobilized) while in the hospital. Activity is very important in COPD management.
- Smoking cessation often is not addressed in the hospital and therefore education and medications to aid in successful cessation may not be provided. Thus smokers will most likely re-start smoking as soon as they get home.
- Prior to discharge, intravenous medications may not be adequately converted to oral medications with instructions for administration at home.
- Patient training for long-term management of COPD has not begun.
Discharge/transition to home care:
- Acute exacerbations often require more than the 3-5 day length of stay for resolution. This can leave the patient vulnerable to relapse if the treatment is interrupted or inadequately continued at home.
- Intravenous medications may not be converted to oral medications before discharge.
- Inhaled medications may still be administered through nebulizers and not converted to meter-dose inhalers, and/or nebulizers may not be provided for home administration of bronchodilators.
- Interruption of medication between in-patient and home care.
- Medications may not be available at home.
- Medication administration instruction may be inadequate.
- No follow-through on smoking cessation plan, including medication adherence.
Home care COPD management – finish exacerbation treatment and proceed to address the chronic component.
- Inadequate outpatient management assuring that the exacerbation is fully resolved.
- Inadequate training for managing the chronic component of COPD.
- Inadequate medication and/or training on medication administration.
- Failure to reconcile home medications prescribed by different providers.
- Inadequate instruction on proper airway clearance.
- Inadequate titration of home oxygen and portable oxygen devices.
- Inadequate monitoring of oxygen saturation.
- Sedentary lifestyle resulting in inadequate mobilization
- Re-started smoking at home.
- Inadequate home care monitoring.
- Lack of follow-up physician appointment.
A COPD exacerbation is a dynamic process leading to destruction and airway remodeling. Thus it is time sensitive (time is tissue). When destruction occurs, repair takes longer, tissue may not fully repair. This can lower the baseline status, rendering a future exacerbation more likely.
CONCLUSION
A COPD exacerbation is a serious event that can be disabling and even life threatening. Prevention as well as proactive intervention at the first sign of an exacerbation is important. The keys to success are making sure there is early recognition of the exacerbation, avoiding delays in treatment, and treating with adequate intensity. Often we do not see the exacerbation through to resolution, thus leaving an active process smoldering. Post exacerbation, these patients should be monitored more regularly since a previous exacerbation portends the next exacerbation.
REFERENCES
- Rau, J. A Guide to Medicare’s Readmissions Penalties and Data. Kaiser Health News. Oct 2, 2014
- Hoyert DL, Xu JQ. Deaths: preliminary data for 2011. Natl Vital Stat Rep. 2012;61(6):1-65
- Jenks S, Williams M, Coleman E. Re-hospitalization among patients in the Medicare fee-for-service program. N Eng J Med. 2009; 360:14
- Carlin BW, Wiles K, Easley D. Transition of Care and Rehospitalization Rates for Patients Who Require Home Oxygen Therapy Following Hospitalization.
Eur Respir J. 2012; 40(Meeting Abstracts):P617 - Tiep B, Barnett M, Carter R; Lifetime management of COPD via a Clinical Guidance System: 12th year of a continuous care model. Am J Respir Crit Care Med. 189;2014:A1910
- Young MS, Craddock KM et al. COPD training by respiratory care practitioners decreases healthcare utilization and improves patient outcomes. Am J Respir Crit Care Med. 189;2014:A5943
- Calkins, DR, Davis, RB, Reiley, P et al. Patient-physician communication at hospital discharge and patients’ understanding of the postdischarge treatment plan. Arch Intern. Med. 1997; 157: 1026–1030
- Tiep B. Disease management of COPD with pulmonary rehabilitation. Chest. 1997;112:1630-1656
- Tiep BL. In: Celli B, McNee W. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J. 2004; 23: 932–946
- Tiep B, Barnett M. Disease management for chronic obstructive pulmonary disease, A clinical approach. Dis Manage Health Outcomes. 2008:16(5):305313
- Tiep BL, Burns M, Kao D, Madison R and Herrera J. Pursed lips breathing training using ear oximetry. Chest. 1986; 90:218-221
