Michael Neal, CRNA, MSN, Anesthesia Clinical Team Leader, EP Lab Duke University Medical Center, Department of Anesthesiology, Durham, North Carolina
Ablations are performed to treat multiple types of cardiac arrhythmias, ranging from atrial fibrillation to ventricular tachycardia. Ablation procedures improve the lives of individuals who are either unresponsive to anti-arrhythmic medications or for whom the side effects of medications are not tolerable. These cardiac ablations, performed in the electrophysiology (EP) lab, are not without risk to the patient. Providers in the EP lab attempt to minimize these risks, but they are not completely eliminated. Several major risks associated with cardiac ablations are cerebral vascular accident (CVA), neurological compromise from lack and/or low blood perfusion to the brain, and respiratory acidosis related to the accumulative build-up of carbon dioxide. Anesthesia providers in the EP lab anesthetize and sedate patients for ablation procedures and monitor the patient’s vital signs, helping to detect and minimize some of these potential physiological complications. One important resource anesthesia providers can utilize to help identify and minimize the impact of these conditions is the near-infrared spectroscopy (NIRS) cerebral oximeter.
NIRS cerebral oximetry is a noninvasive, continuous monitor which measures the oxygen saturation within the tissue of the brain. This technology has been widely adopted in cardiovascular, carotid and pediatric surgery arenas since the introduction in the early 1990s. Growing areas of clinical applications include neurosurgery, beach-chair positioned surgery, intensive care monitoring and other settings or procedures in which the brain is at risk of hypoxia. Bilateral monitoring of the hemispheres is available and can be displayed real-time, making the cerebral oximeter an invaluable addition to the patient monitoring armature in the EP lab. Using the cerebral oximeter, an EP anesthesia provider can monitor for the development of a clot-related stroke, brain perfusion affected by low or absent blood pressure, and cerebral vessel dilation due to carbon dioxide accumulation.
Device Description
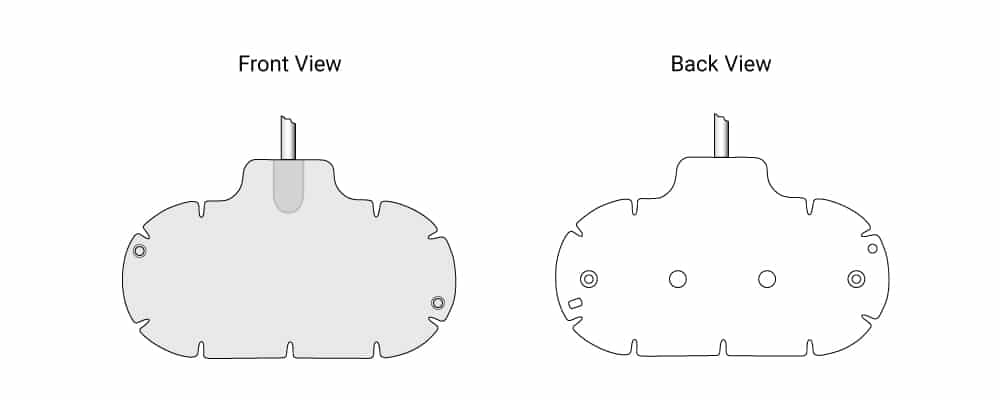
The Equanox™ 7600 system (Nonin Medical, Inc., North Plymouth, MN) utilizes a patented technology with a dual emitter and detector sensor topology (Figure 1). Conventional NIRS cerebral oximeters use a single emitter and two detectors for the optical measurements, where measurements from the shorter path (extracranial saturation) are subtracted from the longer path (intracranial and extracranial saturation) to give intracranial oxygen saturation. The unique architecture of the Equanox sensors allows for further reduction of the effect of surface and shallow tissue variations. Additionally, Equanox technology includes specialized shielding and advanced signal processing to improve signal quality and stability, especially valuable in environments such as the electrophysiology laboratory where high voltage is inherent and risk of electrical interference is significant.
Clinical Applications
Invasive cardiac procedures, such as cardiac ablations, have an inherent risk of thrombus development and possible CVA, especially when large blood vessels are cannulated to insert catheters into the heart. Ablation procedures utilize large vein and sometimes arterial sheaths to introduce EP catheters into the heart, thereby placing the patient at risk for a CVA. This is especially true when there are multiple catheters and/or when an ablation procedure is lengthy. Intravascular sheaths are flushed and heparin therapy may be utilized to minimize clot formation, but at any given moment, a clot could form. This would either travel to the lungs or to the brain if there is a patent pathway from the right to the left side of the heart. The trans-septal procedures during an ablation raise the CVA risk even higher when a temporary septal hole is created in order to access the left side of the heart. Thrombi present in the venous system could then travel through this access in the septal wall and then to the brain.
If cerebral oximetry is used in the EP lab, the quality of perfusion to both brain hemispheres will be displayed in real-time, allowing an anesthesia provider to see if cerebral blood supply is compromised and intervene appropriately. A dramatic unilateral change in values (i.e., one of two cerebral oximetry numbers displayed drops independently) might indicate a CVA formation in one side of the brain. A bilateral drop in figures is more indicative of a low blood pressure/hemodynamic state. It could also indicate that clots might have formed, which could have a more global effect on cerebral perfusion. If the patient is receiving mild conscious sedation for their procedure and is able to speak, providers might notice a change in speech quality and/or gross motor control. However, many times patients require general anesthesia and are intubated or receive heavy sedation, which prevents them from interacting with the anesthesia provider. Thus, the cerebral oximeter can aid in the detection of neurological compromise from a thrombus related CVA. In this instance, the ablation could be aborted, and interventions such as a CT scan and interventional therapy could be initiated much sooner due to the early detection with the cerebral oximeter.
Another risk related to ablation procedures is a potential neurological insult from lack of proper blood flow to the brain caused by prolonged hypotension. Commonly, patients who require an ablation have an arrhythmia, such as ventricular tachycardia, that can symptomatically lower their blood pressure. When a patient is undergoing an ablation procedure, the arrhythmia needs to be induced in order to locate the origin of the arrhythmia and determine where the ablation burn should occur. Inducing some types of arrhythmias requires either fast pacing via an EP pacing catheter (rates of 200 bpm or higher) or inducement by medications. One such medication is isoproterenol (Isuprel), a potent beta-1 agonist that has the ability to generate rapid heart rates due to its positive chronotropic effect. Regardless of the inducement type, a high heart rate alone can drop the blood pressure and the patient’s cerebral perfusion pressure. Then, if the unwanted arrhythmia is induced, the patient can be further compromised if the blood pressure is lowered for a significant amount of time and cerebral perfusion pressures fall below baseline values. Drops in blood pressure can be severe during an ablation case (such as during VT ablation), when pressures drop below 60 mmHg. These drops can be transient in nature as the induced arrhythmia can be corrected either by pacing or by DC cardioversion. Medications such as vasopressors are sometimes given to help stabilize a patient’s blood pressure during these periods, but due to the extreme drop from baseline (sometimes to the point of complete pulselessness), it is vital for the EP team to react quickly. If a cerebral oximeter is being utilized during these situations, the anesthesia provider can quickly notify the EP surgeon that the arrhythmia is compromising cerebral blood flow. Of note is the fact that the cerebral oximeter does not depend on pulsatile flow and is able to provide accurate monitoring regardless of the perfusion status and pulse status. This is extremely useful if there is no arterial line to monitor blood pressure values and the blood pressure has dropped significantly, making non-invasive monitoring difficult.
Patients may also respond differently to drops in blood pressure. An older patient with undiagnosed carotid plaques and possible partial carotid artery obstruction may need a higher baseline blood pressure to maintain proper cerebral pressure. When a significant drop in blood pressure occurs during an ablation, these patients are at greater risk of neurological compromise. Even a small drop from baseline blood pressure may be symptomatic in terms of maintaining proper cerebral perfusion. This patient will most likely be under general or heavy IV sedation, and the EP team will not be able to identify potentially crucial drops in cerebral blood flow unless a cerebral oximeter is being used. Cerebral perfusion allows the clinician to assess the adequacy of the blood pressure for individual patients by directly interrogating the adequacy of perfusion of the brain. Patients may also take longer to recover cerebral perfusion from hypotensive events in the EP lab. The anesthesia provider, having the cerebral oximeter to help guide their care, can inform the EP team when the patient has restored their cerebral blood flow back to baseline levels. This is important for longer EP cases, some of which can last up to ten hours or more. Anesthesia providers, who utilize the benefits of cerebral oximetry in the EP lab, will be able to monitor the effects of unstable blood pressures on cerebral perfusion versus not knowing an anesthetized patient’s neurological status until the end of the case.
A third potential use of the cerebral oximeter in the EP lab is to indirectly monitor for cerebral dilation related to increased arterial carbon dioxide levels (PACO2). Ablations under a general anesthesia (intubated/mechanically ventilated) often require “breath holding” to minimize intra-thoracic changes related to breathing. EP surgeons will request that mechanical ventilation be stopped temporarily to minimize thoracic movement and unwanted movement of EP catheters that can be seen during fluoroscopy of the heart during the ablation process. Breath holding does present its own list of problems, mainly limiting proper CO2 exchange (and PAO2 if holding is prolonged). Anesthesia providers may try to offset the change to PAO2 by increasing oxygen mixture to 100% FIO2. This may “buy some time” before a provider sees a change in pulse-oximeter, but PACO2 will continue to rise, sometimes to critical levels, causing respiratory acidosis. A provider might notice that cerebral-oximeter numbers rise due to the accumulation of PACO2. At times, breath holding can last from 2–3 minutes, and the anesthesia monitor will not be able to measure end-tidal CO2 unless there is active breathing. A rapid rise in cerebral-ox numbers above baseline might indicate that CO2 has caused cerebral vasodilation and that breathing should occur to restore CO2 back to baseline values. CO2 increase can be problematic for the EP patient when breath holding occurs many times over a long case time. Anesthesia providers do have the option of processing an arterial blood sample (ABG), but this can be costly if repeated samples are sent to the lab. ABGs may also be difficult to obtain if the patient does not have arterial access and the patient is fully draped and sterile in a typical EP manner. EP surgeons may request, after a prolonged mechanical breath hold, to have ventilations held again, before enough time was given to ventilate the patient and re-establish proper arterial gas levels. Providers may only get a “snap-shot” of the end tidal CO2 value and might not be able to see a slow, but definite rise in values until the CO2 reaches a critical value (70 or higher). Utilizing the cerebral oximeter gives a provider the ability to chart an upward rise in CO2 and to identify the need to restart patient ventilation.
Conclusion
The ultimate goal of ablation therapy is to restore or improve cardiac function by eliminating unwanted cardiac rhythms. This goal should be achieved without sacrificing brain function due to prolonged low cerebral perfusion pressure or the occurrence of a CVA during an ablation procedure. One way EP labs can help lower the risks associated with ablations is to use a cerebral oximeter. The cerebral oximeter can act as a watchdog during an ablation by monitoring cerebral perfusion and detecting possible stroke formation. By using a cerebral oximeter, anesthesia providers can help the EP team plot the next course of action needed to protect the patient from harm during cardiac ablations (i.e., when to terminate an induced arrhythmia such as ventricular tachycardia). Providers who use the cerebral oximeter also have peace of mind knowing that a patient is receiving proper cerebral perfusion during an ablation, especially when hemodynamically altering arrhythmias are generated. Providers can also use the oximeter to detect cerebral vasodilation from carbon dioxide accumulation and make appropriate changes to prevent acidosis. The cerebral oximeter has the potential to become a standard monitor for high-risk cases such as cardiac ablations, just as the pulse oximeter became a standard monitor in all anesthetic cases. There is an ongoing effort to incorporate new and updated ablation technologies in the EP lab, such as new cardiac mapping techniques, and there should also be an effort to improve patient monitoring as well. Cerebral oximetry is a good example of how providers can employ new technology to improve the overall outcome of procedures and raise the standard in patient care.
References
- Cohen TJ. Practical Electrophysiology. PA: HMP Communications, 2005.
- Steinberg JS. Electrophysiology: The Basics. A Companion Guide for the Cardiology Fellow during the EP Rotation. MD: Lippincott Williams & Wilkins, 2009.
- Zipes DP , Jalife J. Cardiac Electrophysiology: From Cell to Bedside. PA: Saunders, 2009.
