How Do I Know if My Pulse Oximeter is Accurate?
With the widespread, almost ubiquitous use of pulse oximeters, it is a question that is often asked. It is a question that should be asked, particularly with the proliferation of inexpensive devices on the market. How do you know if your pulse oximeter is accurate and why is there variability between manufacturers’ devices? When compared side by side, does a higher number necessarily mean that device is more accurate? This paper examines how pulse oximeters are calibrated, the difference between accuracy and bias and what you need to know about your pulse oximeter.
How are Pulse Oximeters Calibrated?
To answer this question, it is important to first understand that all pulse oximeters are calibrated using CO-oximeters, which are widely assumed to represent the truth. Pulse oximeter manufacturers conduct highly structured clinical trials that induce hypoxia in healthy adult subjects. Arterial blood samples taken at precise intervals are analyzed on a CO-oximeter (direct measurement) and used as references for the calibration of the pulse oximeter (noninvasive indirect measurement). Both methods are used to determine the concentration of oxygen bound to hemoglobin in the blood. CO-oximeters are heavily used in clinical laboratories of hospitals and other clinical settings, but a blood sample is always required and must be properly handled to ensure an accurate result.
What is Bias?
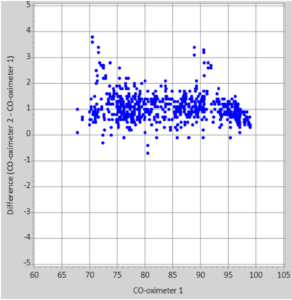
There are many CO-oximeters on the market and they generally will provide the same results. However, like most measurement equipment, CO-oximeters are not perfect and have an inherent bias to their measurements. This means that the same blood sample analyzed by multiple CO-oximeters may give results that differ by as much as 2–3% between two devices. This bias can be seen between CO-oximeter manufacturers as shown in Figure 1. This example shows two CO-oximeters measuring the same samples of oxygenated hemoglobin at different oxygen concentrations. For most concentrations of oxygen, CO-oximeter 2 reads approximately 1% higher than CO-oximeter 1. While both CO-oximeters are accurate, each has its own bias.
Why is There Variability Between Pulse Oximeters?
There are several reasons that different manufacturers’ pulse oximeters give different readings on the same person, starting with the calibration. Using the example in Figure 1, calibrating a pulse oximeter to CO-oximeter 2 would yield a device that reads a higher SpO2 than a pulse oximeter calibrated to CO-oximeter 1. Both devices may still be accurate but will have a high or low bias based on which CO-oximeter was used for calibration. In addition, each pulse oximeter manufacturer has its own accuracy specifications with different sensors and at different oxygen saturations. This accuracy – known as Arms – is typically between 1% and 3% and contributes to the variability between devices from different manufacturers.
Does a Higher SpO2 Reading Mean My Pulse Oximeter Is More Accurate?
No. This may be a result of high bias. Being biased high raises an additional important question: Should a pulse oximeter read 100% on a patient breathing room air? Oxygen saturation of the blood is determined by the amount of oxygen in arterial blood and how many sites oxygen can bind to on the hemoglobin molecule. At sea level, 21% of air is made up of oxygen which can also be converted to a pressure (atmospheric pressure is 760 mmHg; therefore, 21% of 760 = 160 mmHg).1 (At higher altitudes, the atmospheric pressure is reduced and therefore would exaggerate this example further.) In theory, all inhaled oxygen should bind to a hemoglobin molecule, but due to physiologic inefficiencies during respiration, the actual partial pressure of oxygen in arterial blood (PaO2) is between 90–100 mmHg.2 Examining the oxyhemoglobin dissociation curve (Figure 2), at a PaO2 of 100 mmHg (room air), not all hemoglobin
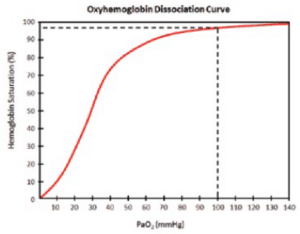
binding sites are occupied. Most healthy individuals have an SpO2 reading between 95 and 100% in room air so pulse oximeters that read 100% at room air may be biased high. A high bias can cause significant delays in treatment when treatment thresholds are reached. Most importantly, pulse oximeter readings that are close to an intervention threshold should always be used in conjunction with other methods of patient assessment and not used as the sole determinant of when to take action.
How is Nonin Medical’s PureSAT® Pulse Oximetry Technology Calibrated and Why is it Different?
Nonin Medical uses the most current CO-oximeter technology to calibrate its full range of pulse oximeters. In clinical hypoxia studies, Nonin follows a strict protocol in which multiple samples are taken at each SpO2 interval and handled with extreme care and precision to ensure accurate calibration to the CO-oximeter. When incorporated into the design of a Nonin Medical pulse oximeter, this results in consistent, repeatable measurements in a variety of clinical settings on a broad range of patients. Nonin Medical’s clinically- proven PureSAT pulse oximetry technology utilizes intelligent pulse-by-pulse filtering to provide precise oximetry measurements — even in the presence of motion, low perfusion, dark skin tones and other challenging conditions. By reading the entire plethysmographic waveform, PureSAT signal processing pre-filters the pulse signals to remove undesirable signals. Advanced algorithms then separate the pulse signals from artifact and interference — leaving only the true pulse. And with Nonin’s smart averaging technology, PureSAT automatically adjusts to each patient’s condition to provide fast and reliable readings you can trust.
